
Although many view a colonoscopy as an uncomfortable or even scary procedure, 17.7 million of them are carried out annually in the United States, and 60.6 percent of people aged 50 to 75 without a personal history of colorectal cancer have had one in the past 10 years.
It’s believed that a colonoscopy not only helps find cancer but also prevents cancer from developing from polyps. Because of its high level of sensitivity and specificity, colonoscopies have been regarded as the gold standard for colon cancer screenings for a long time.
Unexpected Result From a Major Colonoscopy Study
However, a recent major clinical study, the Nordic-European Initiative on Colorectal Cancer (NordICC) study published in October 2022, raised questions about the efficacy of colonoscopies.
The study suggested that colonoscopies don’t save as many lives as previously thought.
Researchers recruited 84,585 participants in Poland, Norway, Sweden, and the Netherlands; 28,220 were in the invited group (invited to have a colonoscopy), and 56,365 were in the usual-care group.
At the end of the 10-year follow-up, the risk of colorectal cancer-related death at 10 years was 0.28 percent among participants in the invited group and 0.31 percent in the usual-care group. The risk of death from any cause was 11.03 percent in the invited group and 11.04 percent in the usual-care group.
In terms of adverse events, 15 people had major bleeding after polyp removal. According to the study, there were no screen-related deaths within 30 days after colonoscopy.
The incidence of colon cancer has dropped significantly since 1975. Most people believe that this is due to increased screening and improved treatment.
Since there were no randomized clinical trial data on colonoscopies for colorectal cancer before, the NordICC trial sparked a heated discussion: Can colonoscopies truly prevent colon cancer?
If the benefit isn’t what people have expected, the colon cancer-screening landscape could be totally reshaped.
The Study Invokes Intense Debate
Doctors perceive the results of the NordICC study differently for the following reasons.
First, the trial had lower-than-expected participation—only 42 percent underwent colonoscopy—and provides no information on adherence to guidelines for polyp surveillance.
Most think the study doesn’t change the value of colonoscopies. The test would’ve lowered cancer risk by 31 percent and cut the probability of dying from colorectal cancer by 50 percent if compliance had been 100 percent, according to the research findings.
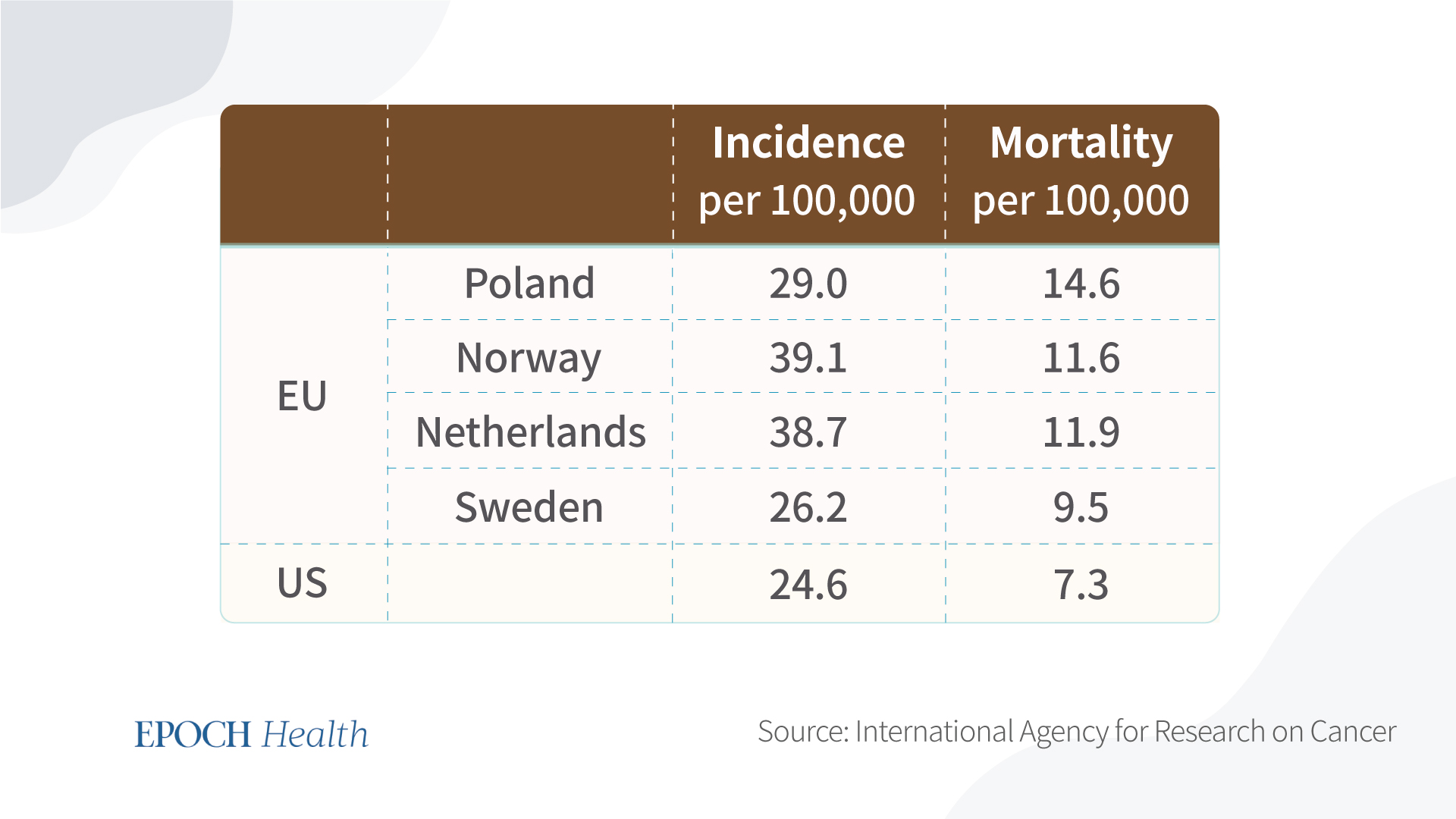
Also, the tested countries have a higher mortality rate and incidence rate compared to the United States. U.S. clinicians favor colonoscopies, while European health systems rely far more on flexible sigmoidoscopy, which only examines the lower part of the colon.
Second, the operator affects the colonoscopy’s effectiveness. The adenoma detection rate is the percentage of screening colonoscopies in which one or more adenomas are found.
Patients are better protected from adenoma development by endoscopists with higher adenoma detection rates.
Third, the study was done among European populations and may not be representative of the various demographics in the United States.
The Risks of Colonoscopy
The benefits and risks depend on compliance with the screening protocol, the chance of meeting with an experienced endoscopist, and your own risk of developing colon cancer.
On the other hand, a healthy lifestyle doesn’t guarantee that you won’t have colorectal cancer. First-degree relatives of people with colorectal cancer are at a sixfold increased risk of colon cancer before 50 years old. Second- and third-degree relatives correspond to 1 1/2 and three times increased risk, a two- to threefold increased risk of colorectal cancer.
A doctor may determine that you’re at high risk if you have a family history of colon cancer or you have a history of colon polyps or inflammatory bowel disease.
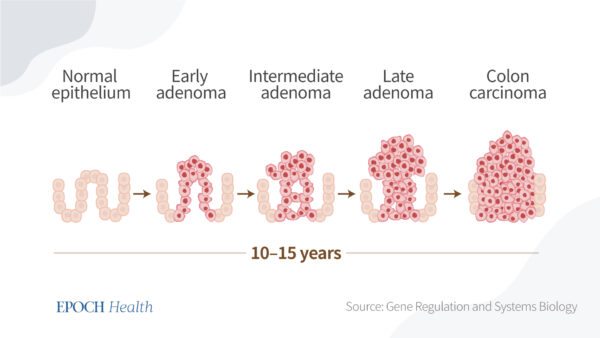
Colonoscopies are still the gold standard if cancer is suspected in a patient. And it will benefit patients most if a cancer is found and removed in the adenoma-carcinoma sequence (the development of cancerous change in a dysplastic polypoid lesion).
The prognosis of patients with colorectal cancer varies according to the site of cancer, with right-sided tumors having the most severe prognosis, making an early diagnosis in this group of patients especially important.
However, there are many risks for colonoscopies—in addition to the risk of sedation.
A colonoscopy is more invasive and burdensome than other colon cancer tests, such as fecal testing and sigmoidoscopy, and it requires more clinical resources.
A few medical organizations have dropped the recommended age to begin colorectal cancer screening to 45 from 50. The reason for this is that scientists are striving to learn more about the causes, the biology, and how to prevent the illness from developing earlier in life. Several risk factors have become more prevalent over the past 45 years, such as obesity, sedentary lifestyles, and smoking, which can lead to more instances of early-onset cancers. Poor diet, particularly one high in processed meat and fat and low in fruits and vegetables, is increasingly being linked to early-onset colorectal cancer. Several studies have also discovered that being overweight or obese may increase one’s risk of developing colorectal cancer with early onset.
Since colorectal cancer is still relatively rare, affecting less than 1.8 per 100,000 younger adults (below age 40), lowering the screening age might be a burden and not cost-effective. In addition, the trend of new young patients might be because of early screening and overdiagnosis, which could further burden the person.
The below figure shows the long process of colon cancer development. If the in situ cancer is identified very early, the five-year survival rate may improve. But no one can really tell how long it takes for a cancer cell to grow into something lethal, and there are other risks to consider that may affect outcomes, as well.
Weigh Both Sides
Deciding whether it’s cost-effective to do a colonoscopy will be based on your own risk of developing colorectal cancer, depending on your family history and other risk factors.
If you develop severe bleeding due to receiving an endoscopy, harm is 100 percent likely. To avoid the chance of harm, or if you can’t tolerate a colonoscopy, some studies have proven that a fecal immunochemical test for screening patients at increased risk for colorectal cancer has high overall diagnostic accuracy, given its safety, simplicity, low cost, accuracy, and minimal discomfort.
We still need better data on a colonoscopy’s benefits and risks. To account for comorbidities, oncological treatments, stage-related differences at the time of diagnosis, family history, and other risk factors, additional in-depth patient-level data are required.
Ideally, when a patient sees a doctor, the doctor would provide him personalized advice; for example, “Mr. Smith, your chance of getting colorectal cancer is X percent based on all the information you’ve provided.”
However, there are many uncertainties in life. Even in the way you cook, what ingredients you use, and how they were processed—it’s hard to digitize such factors, as there’s no single model to predict a person’s risk. Tailoring colorectal cancer screening approaches to each person based on their risk factors and precision screening may improve the efficiency and cost-effectiveness of colonoscopy screening.
Important Notice: This article was originally published at www.theepochtimes.com by Yuwei Zhang, MD, Ph.D., MPH, MBA where all credits are due.
Disclaimer
The watching, interacting, and participation of any kind with anything on this page does not constitute or initiate a doctor-patient relationship with Dr. Farrah™. None of the statements here have been evaluated by the Food and Drug Administration (FDA). The products of Dr. Farrah™ are not intended to diagnose, treat, cure, or prevent any disease. The information being provided should only be considered for education and entertainment purposes only. If you feel that anything you see or hear may be of value to you on this page or on any other medium of any kind associated with, showing, or quoting anything relating to Dr. Farrah™ in any way at any time, you are encouraged to and agree to consult with a licensed healthcare professional in your area to discuss it. If you feel that you’re having a healthcare emergency, seek medical attention immediately. The views expressed here are simply either the views and opinions of Dr. Farrah™ or others appearing and are protected under the first amendment.
Dr. Farrah™ is a highly experienced Licensed Medical Doctor certified in evidence-based clinical nutrition, not some enthusiast, formulator, or medium promoting the wild and unrestrained use of nutrition products for health issues without clinical experience and scientific evidence of therapeutic benefit. Dr. Farrah™ has personally and keenly studied everything she recommends, and more importantly, she’s closely observed the reactions and results in a clinical setting countless times over the course of her career involving the treatment of over 150,000 patients.
Dr. Farrah™ promotes evidence-based natural approaches to health, which means integrating her individual scientific and clinical expertise with the best available external clinical evidence from systematic research. By individual clinical expertise, I refer to the proficiency and judgment that individual clinicians acquire through clinical experience and clinical practice.
Dr. Farrah™ does not make any representation or warranties with respect to the accuracy, applicability, fitness, or completeness of any multimedia content provided. Dr. Farrah™ does not warrant the performance, effectiveness, or applicability of any sites listed, linked, or referenced to, in, or by any multimedia content.
To be clear, the multimedia content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health providers with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read or seen in any website, video, image, or media of any kind. Dr. Farrah™ hereby disclaims any and all liability to any party for any direct, indirect, implied, punitive, special, incidental, or other consequential damages arising directly or indirectly from any use of the content, which is provided as is, and without warranties.








