Magnesium is an essential mineral that is critical for health. It plays a role in a wide variety of body functions including the formation of DNA, bone formation, and the regulation of nerve and muscle function. Low levels have also been linked to the development of depression.
Magnesium and the Brain
In the brain, magnesium helps to regulate the actions of N-methyl-D-aspartate (NMDA) glutamate receptors. These receptors are believed to play an important role in memory formation and learning.
Glutamate is an excitatory neurotransmitter that is important for normal function in the brain. In excess, however, it can cause cells to become overstimulated. This overexcitation of cells ultimately leads to cell death and is linked to conditions such as seizures, stroke, Parkinson’s disease, multiple sclerosis, Alzheimer’s disease, and amyotrophic lateral sclerosis (ALS).
In addition to contributing to these neurological conditions, excessive glutamate activity is also linked to depression and anxiety.
Magnesium blocks the actions of glutamate in the NMDA receptors. If your body is magnesium deficient, it means that few of the NMDA receptors are blocked. This may lead to overexcitation and cell damage. Because of this, it is possible that magnesium may be useful in the treatment and prevention of depression.
Since magnesium plays such an important role in health, a deficiency in this important nutrient could potentially predispose people to a number of different health problems, including depression.1
Magnesium and Depression
Depression is one of the most common mental illnesses and a leading cause of disability worldwide. It contributes to a decreased quality of life and a greater risk of death.
It also commonly co-occurs along with other neurological and chronic pain conditions. Because these are also linked to changes in glutamate activity, it is possible that low magnesium levels may be linked to both the psychiatric and neurological symptoms.1
Treatments for depression often center on psychotherapy and medications, which have been well-validated with a proven record of effectiveness. However, dietary interventions for depression have also been the subject of interest in recent years.
The hope of such research is to find ways that diet and nutritional supplements might be used to prevent or alleviate symptoms of depression. Vitamins and nutrients such as B-vitamins, S-adenosylmethionine (SAMe), 5-hydroxytryptophan (5-HTP), magnesium, and omega-3 fatty acids have all been implicated for possible therapeutic or preventive potential.2
Research on Magnesium for Depression
While promising, the exact effects of dietary magnesium on depression are not yet well understood. There is research that supports the potential use of magnesium supplementation for depression:
- A 2015 study found a significant link between low magnesium intake and depression in adults.3
- A 2017 randomized clinical trial published in the journal PLoS One found that supplementation with magnesium chloride resulted in significant improvements in depressive symptoms.4 The study also found that the participants who were taking an antidepressant experienced stronger benefits when taking magnesium, which suggests that it might be useful when used in conjunction with antidepressant medications.
- A 2019 study found that low serum magnesium levels were associated with depressive symptoms.5 Such findings suggest that measuring magnesium levels may be useful as a way to identify people who might respond best to magnesium supplementation.
One benefit of magnesium as a treatment option is that it is relatively affordable, fast-acting, and well-tolerated by most people.
Reasons You Might Be Magnesium Deficient
While magnesium is critical for health, magnesium deficiency is surprisingly common.
- Dietary magnesium often comes from plant sources. However, magnesium levels can vary depending on how much of the substance the plants absorb from their environment. Environmental factors can, therefore, play a role in how magnesium-rich certain foods are.6
- Other dietary factors can affect magnesium absorption. The use of antacids or diuretics and the consumption of alcohol and caffeine can affect how much magnesium people absorb from the foods they eat.
- Excessive stress can also play a role in depleting magnesium from the body. During times of stress, magnesium is released into blood cells and eventually excreted by the kidneys. While this can initially play a role in protecting the body from some of the negative effects of stress, longer-lasting periods of chronic stress can lead to magnesium depletion and deficiency if this loss is not replaced by dietary consumption.7
- Different forms of magnesium may affect magnesium levels. The type of magnesium supplement used can also affect how readily it is absorbed by the body. Some supplement options tend to be more bioavailable, while others may be more difficult for the body to absorb.
How to Increase Your Magnesium Levels
The average daily recommended amounts of magnesium vary depending on factors such as sex, age, pregnancy, and breastfeeding.
The daily recommended amount for adult men is between 400 and 420 mg and the daily recommended amount for adult women is between 310 and 320 mg per day.8
While magnesium is an essential nutrient, many people do not get enough each day. Certain medical conditions can also make it more likely to become magnesium deficient including celiac disease, type 2 diabetes, and long-term alcohol use disorders.
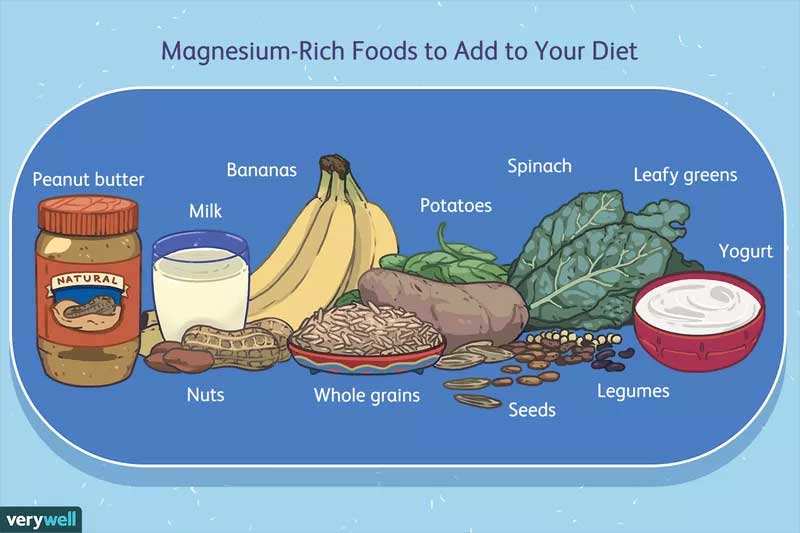
If you want to increase your magnesium intake, one of the best things you can do is to eat a diet that contains foods that are high in magnesium. These include:
- Bananas
- Magnesium-fortified foods
- Legumes
- Milk
- Nuts
- Peanut butter
- Potatoes
- Seeds
- Spinach and other leafy green vegetables
- Whole grains
- Yogurt9
You may also consider taking a magnesium supplement, although you should always discuss this with your doctor first.
Also be sure to tell your doctor about any medications, supplements, or substances that you are also taking before you begin taking magnesium supplements. Some medications, including antibiotics and diuretics, can sometimes create drug interactions if taken with magnesium.
You should also always be sure to only take the amount that your doctor recommends. Very high intakes of magnesium may lead to abdominal pain, diarrhea, and nausea. In some cases, it can lead to heart problems if taken in extremely high doses.8
A Word From Verywell
While the current research shows promise, further research is still needed to explore the use of magnesium as a tool to prevent, alleviate, or treat depression.
Even though more research is needed, you can make sure that you are getting the magnesium you need by eating a healthy, nutritious diet that includes magnesium-rich foods. If you are concerned that you might have a magnesium deficiency or are experiencing symptoms of depression, be sure to talk to your doctor.
Sources:
- Kirkland AE, Sarlo GL, Holton KF. The role of magnesium in neurological disorders. Nutrients. 2018;10(6):730. doi:10.3390/nu10060730
- Rechenberg K. Nutritional interventions in clinical depression. Clinical Psychological Science. 2016;4(1):144-162. doi:10.1177/2167702614566815
- Tarleton EK, Littenberg B. Magnesium intake and depression in adults. The Journal of the American Board of Family Medicine. 2015;28(2):249-256. doi:10.3122/jabfm.2015.02.140176
- Tarleton EK, Littenberg B, MacLean CD, Kennedy AG, Daley C. Role of magnesium supplementation in the treatment of depression: A randomized clinical trial. Song Y, ed. PLoS ONE. 2017;12(6):e0180067. doi:10.1371/journal.pone.0180067
- Tarleton EK, Kennedy AG, Rose GL, Crocker A, Littenberg B. The association between serum magnesium levels and depression in an adult primary care population. Nutrients. 2019;11(7):1475. doi:10.3390/nu11071475
- Guo W, Nazim H, Liang Z, Yang D. Magnesium deficiency in plants: An urgent problem. The Crop Journal. 2016;4(2):83-91. doi:10.1016/j.cj.2015.11.003
- Cuciureanu MD, Vink R. Magnesium and stress. In: Vink R, Nechifor M, editors. Magnesium in the Central Nervous System [Internet]. Adelaide (AU): University of Adelaide Press; 2011.
- National Institutes of Health. Magnesium. Published March 24, 2020.
- Cleveland Clinic. Magnesium-rich food. Reviewed November 24, 2020.
Important Notice: This article was originally published at www.verywellmind.com by Kendra Cherry where all credits are due. Medically reviewed by Daniel B. Block, MD.
Disclaimer
The watching, interacting, and participation of any kind with anything on this page does not constitute or initiate a doctor-patient relationship with Dr. Farrah®. None of the statements here have been evaluated by the Food and Drug Administration (FDA). The products of Dr. Farrah® are not intended to diagnose, treat, cure, or prevent any disease. The information being provided should only be considered for education and entertainment purposes only. If you feel that anything you see or hear may be of value to you on this page or on any other medium of any kind associated with, showing, or quoting anything relating to Dr. Farrah® in any way at any time, you are encouraged to and agree to consult with a licensed healthcare professional in your area to discuss it. If you feel that you’re having a healthcare emergency, seek medical attention immediately. The views expressed here are simply either the views and opinions of Dr. Farrah® or others appearing and are protected under the first amendment.
Dr. Farrah® is a highly experienced Licensed Medical Doctor certified in evidence-based clinical nutrition, not some enthusiast, formulator, or medium promoting the wild and unrestrained use of nutrition products for health issues without clinical experience and scientific evidence of therapeutic benefit. Dr. Farrah® has personally and keenly studied everything she recommends, and more importantly, she’s closely observed the reactions and results in a clinical setting countless times over the course of her career involving the treatment of over 150,000 patients.
Dr. Farrah® promotes evidence-based natural approaches to health, which means integrating her individual scientific and clinical expertise with the best available external clinical evidence from systematic research. By individual clinical expertise, I refer to the proficiency and judgment that individual clinicians acquire through clinical experience and clinical practice.
Dr. Farrah® does not make any representation or warranties with respect to the accuracy, applicability, fitness, or completeness of any multimedia content provided. Dr. Farrah® does not warrant the performance, effectiveness, or applicability of any sites listed, linked, or referenced to, in, or by any multimedia content.
To be clear, the multimedia content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health providers with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read or seen in any website, video, image, or media of any kind. Dr. Farrah® hereby disclaims any and all liability to any party for any direct, indirect, implied, punitive, special, incidental, or other consequential damages arising directly or indirectly from any use of the content, which is provided as is, and without warranties.








